Your Guide to Chronic Care Management (CCM) CPT Codes & Billing
Without a proper understanding of CCM billing, you can miss out on optimizing revenue for your practice and providing quality care for your patients. In this blog, discover the key elements and requirements for billing the Chronic Care Management (CCM) CPT Codes.
What is Chronic Care Management (CCM)?
CCM was introduced to the United States in 1996 to enhance chronic disease care. These services are generally performed outside the face-to-face context and involve establishing, implementing, revising, or monitoring a care plan for a patient with multiple chronic conditions, including the following:
- around-the-clock access to healthcare advice
- monthly patient consultations
- logistical support for necessities like medication refills and transportation
- timely sharing of health information
- scheduling appointments or services
And yet, more than two decades later, CCM has become more complex than ever, with new CCM codes and requirements to be constantly aware of.
CCM CPT codes you need to know
These CPT codes are generally used to bill CCM services to CMS and are divided into complex and non-complex (also known as basic or standard) CCM services.
While we know that CCM services offer additional support and resources to patients with chronic conditions, your practice may falter from reducing billing stress and patient satisfaction once billing errors occur. Dealing with common errors such as incorrect patient information, wrong CPT codes, and poor claims submission, can take away precious time spent focusing on your patient’s treatment journey. Worse, your practice won’t get paid for the time and effort you invested in caring for them. How can you get ahead of this? Learn the steps for CCM billing below.
How to bill CCM services
Although most CCM services are provided by clinical staff, only one physician with a National Provider Identifier (NPI) number or another qualified healthcare professional can bill them in a given calendar month. For non-physicians, they must be legally authorized and qualified to provide CCM in the state in which the services are furnished. Here’s what you need to do to bill for CCM:
- Patient eligibility verification: Identify Medicare Part B patients with two or more chronic conditions expected to last at least 12 months or until the patient’s death.
- Minimum of 20 minutes of CCM services were provided.
- Claims submission to CMS.
- Patient invoice: Invoice the copay and any other charges for their monthly CCM services.
- Evaluate: Make sure there are no conflicting codes that have been billed.
Read CMS’ Chronic Care Management Services booklet in full to learn more.
However, claim denials may be more common than you think. In 2023, insurers reported receiving 425 million claims, of which 92% (392 million) were filed for in-network services, yet 73 million were denied.
Providers must look for inefficiencies to solve these “claims nightmares.” Clinician and staff burnout may be drivers of these errors. Overworking increases the chances of making mistakes that result in claims denial, decreased payments, and decreased revenues. That’s why it’s best to turn your investment toward outsourcing a billing company that can maximize your profitability and ROI on CCM services.
Closer Look: A Physical Therapy Practice Reaching Heights with Synapse
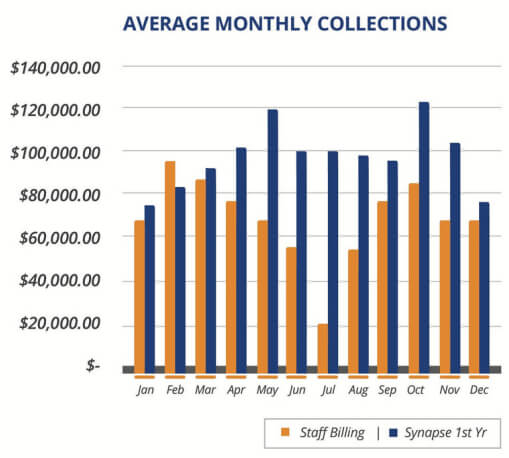
This client came to us with hundreds of claims and struggled to reach $100,000.00 in collections. Since switching to
Synapse Revenue Cycle Management, they have not only exceeded $100,000.00 in monthly collections, but they have also improved their staff billing by 41.46%.
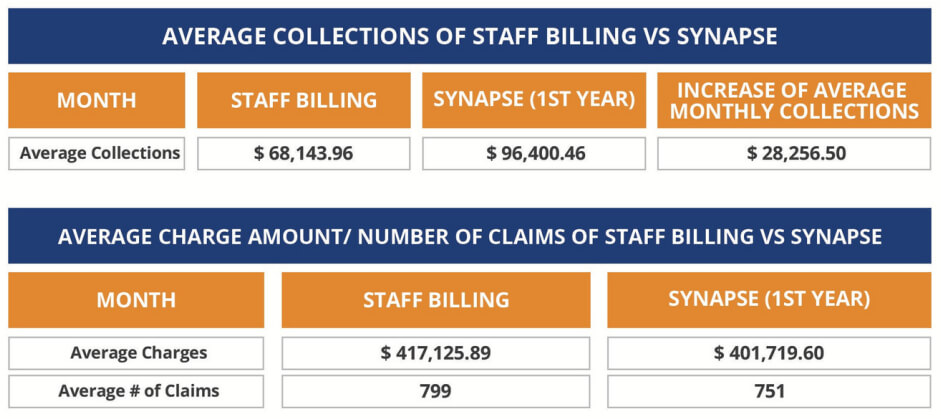
Average charges and average # claims is slightly higher with Staff Billing Compared to Synapse
Synapse has shown for more than 25 years the fruits of handling every single claim with extra care. We reduce duplicative, poorly designed, or unnecessary tasks, so you can be more present in the life-saving work that you do. Most importantly, we take care of every bottom line and front desk needs with high-quality RCM services, such as:
- EMR/EHR: From straightforward billing modules to fully integrated electronic health record systems, with our expertise and guidance, you may improve patient care.
- Coding: To assist you improve the efficiency of your revenue cycle management, Synapse provides extensive coding services.
- Credentialing: Let us manage and track all of your enrollments for you so you can concentrate on providing excellent patient care.
- Collections: From claim submission and tracking to resolving denials and delayed payments, Synapse handles all aspects of your revenue cycle management.
- Software Development: We will work with you to develop a user-friendly, visually appealing, and efficient online presence for your practice.
Our Dashboard system displays the Accounts Receivable data in an organized and efficient manner using common parameters such as age bucket, denials, and payer class, resulting in faster transactions.
Your Chronic Care Management (CCM) has a trusted partner to work with you through every claim – Gain the Synapse experience today!
Source
(2024). Aha.org.
https://www.aha.org/system/files/content/00-10/071204_H4L_FocusonWellness.pdf
Lo, J., Long, M., Wallace, R., Salaga, M., & Pestaina, K. (2025, January 27). Claims Denials and Appeals in ACA Marketplace Plans in 2023 | KFF. KFF.
https://www.kff.org/private-insurance/issue-brief/claims-denials-and-appeals-in-aca-marketplace-plans-in-2023/
